Overview | Clinical Scenarios | References
By Jacob M. Appel, MD, JD
OVERVIEW
Definition
Boundaries are principles designed to maintain the professional, fiduciary nature of the physician-patient relationship. Care should be made to maintain a professional physician-patient relationship at all times and to only cross boundaries when in the interest of the patient.
Boundary crossings
- Any action that crosses a boundary, even if benign or in the patient’s interest.1
- A therapist divulging a small amount of personal information, such as where the therapist went on vacation, is a boundary crossing.
Boundary violation
- A serious boundary crossing that defies norms and laws designed to protect the patient’s welfare that may also result in disciplinary action against providers and even criminal charges.
- Examples of boundary violations might include:
- Sexual contact between a psychiatrist and patient.
- Sexual relationships with key third parties such as patients’ relatives.
- Using proprietary information shared by the patient to invest in the stock
market. - Asking the patient for assistance in securing a favor for a friend or family
member (such as assistance gaining admission to college for a child).
![]()
Context
Boundary crossings may be initiated either by the provider or by the patient. It is the responsibility of the provider to ensure that such crossings do not become violations.
CLINICAL SCENARIOS
Scenario #1: A patient presents a provider with a costly gift. How should the provider handle this situation?
- This might create a conflict of interest and the gift should be politely declined.
- The best approach is to thank the patient for the thought, but clearly explain why the gift cannot be accepted.
- Even if the patient is terminating care, such gifts should still be declined because the patient may wish to resume care and/or may refer friends or colleagues.
- Smaller, “token” items may be accepted under limited circumstances if they are unlikely to impact the care relationship and/or rejecting them might have a negative impact upon the patient. An example might be a drawing or painting made by the patient as part of an art therapy program.
Scenario #2: A provider initiates sexual contact with a patient. Under what circumstances is this permissible?
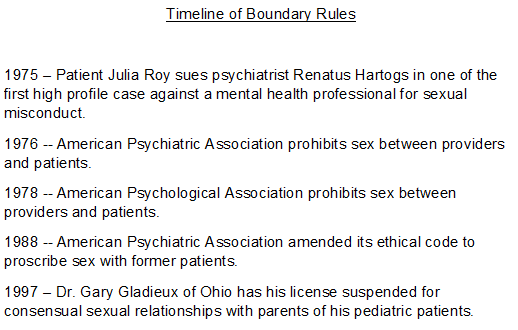
- Psychiatrists may never have sexual or romantic relationships with patients. Arguments favoring this rule rely both upon fears of duress and power inequalities, and also mismanagement of transference leading to poor care.
- APA rules also prevent psychiatrists from having sexual or romantic relationships with former patients. This is a bright-line rule; there are no exceptions.
- Delineating a clear boundary when a patient makes a sexual or romantic advance is essential.
- Any significant boundary violations should be clearly documented in the chart as should the provider’s response. It may sometimes be helpful to contact a superior to make them aware of the situation and to document this action as well
- Rules regarding sexual relationships with former patients vary by specialty, but often include a “wash-out” period between terminating a physician-patient relationship and beginning a sexual one.
- In many jurisdictions, physicians must report previous providers who have had sexual relationships with patients even when the patient objects.2
Scenario #3: A patient tries to befriend a provider through social media. Should the provider accept this offer?
- Generally, no. Such a connection might embroil the provider and patient in an association that is incompatible with the therapeutic relationship and should be declined.3
- Unnecessary entanglement with a patient’s life should be avoided even if the patient just not object to the entanglement.4
- Setting limits for patients who cross boundaries in significant ways is essential for a healthy therapeutic relationship.
- Boundary crossing may lead to boundary violations via a slippery slope: a psychiatrist may drive a patient home after one session, and then meet the patient at a coffee shop for another, and ultimately enter into a prohibited sexual relationship. Social media can prove an insidious gateway to such violations
Slippery Slope Model
- If the patient engages in boundary violations despite significant efforts to delineate appropriate conduct, the provider may choose to refer the patient elsewhere.
- Some minor boundary crossings are benign and may serve the patient’s interests. For instance, a provider may feel comfortable sharing a limited amount of personal information with a patient (such as telling the patient where she is vacationing)
- Whether an action constitutes a boundary crossing or violation is not entirely clear, but physicians should act with caution.5
REFERENCES
- Gabbard GO, Nadelson C. Professional boundaries in the physician-patient relationship. JAMA. 1995 May 10;273(18):1445-9. Available from: https://jamanetwork.com/journals/jama/article-abstract/388355
- MacIntyre MR, Appel JM. Legal and Ethics Considerations in Reporting Sexual Exploitation by Previous Providers. J Am Acad Psychiatry Law. 2020 Jun;48(2):166-175. Available from: http://jaapl.org/content/early/2020/02/12/JAAPL.003911-20
- Cork N, Grant P. Blurred lines: the General Medical Council guidance on doctors and social media . Clin Med (Lond). 2016 Jun;16(3):219-22. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5922698/
- Appel JM. Engagement without entanglement: a framework for non-sexual patient-physician boundaries. J Med Ethics. 2021 Jul 14:medethics-2021-107580. Available from: https://jme.bmj.com/content/medethics/early/2021/07/14/medethics-2021-107580.full.pdf
- Gutheil TG, Gabbard GO. The concept of boundaries in clinical practice: theoretical and risk-management dimensions. Am J Psychiatry. 1993 Feb;150(2):188-96. Available from: https://kspope.com/ethics/boundaries.php
Additional Reading
- Aravind VK, Krishnaram VD, Thasneem Z. Boundary crossings and violations in clinical settings. Indian J Psychol Med. 2012 Jan;34(1):21-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3361837/
- Addressing Sexual Boundaries: Guidelines for State Medical Boards, Federation of State Medical Boards (2006). https://www.fsmb.org/siteassets/advocacy/policies/grpol_sexual-boundaries.pdf
- APA Commentary on Ethics in Practice, Topic 3.2.6 Therapeutic boundary keeping. https://www.psychiatry.org/file%20library/psychiatrists/practice/ethics/apa-commentary-on-ethics-in-practice.pdf
- “Romantic or Sexual Relationships with Patients,” Code of Medical Ethics Opinion 9.1.1, https://www.ama-assn.org/delivering-care/ethics/romantic-or-sexual-relationships-patients