Overview | Clinical Scenarios | Additional Tips | References
By Deborah Giorgi-Guarnieri
OVERVIEW
General Principles
- Abandonment occurs when the psychiatrist does not end the doctor-patient relationship properly.
- Two ways to end a treatment relationship are transfer of care and termination.
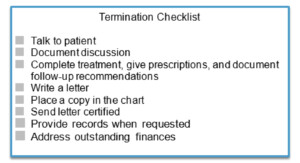
- Ideally, termination should be discussed in person and followed up in writing. If the patient terminates the relationship, then the clinician should follow-up with a letter.
- Proper termination includes reasonable notice, treatment recommendations and education, resources for future treatment, records and information, and a follow-up letter.
Special Considerations
- Acute phase of treatment: Delay ending the relationship until the acute phase of treatment is over. Emergency closing your practice may not end your patient obligations to terminate appropriately.
- Only source of treatment: Consider distance and availability of treatment alternatives prior to terminating the relationship.
- Group practices: Consider discharging the patient from the entire practice if on-call situations may require further clinician-patient contact.
- Protected rights or English proficiency: Examples of civil rights laws include the Civil Rights Act, the Americans with Disabilities Act (ADA), and the Emergency Medical Treatment and Labor Act (EMTALA).
- Patient’s disability: The patient’s disability cannot serve as the reason for termination. If the patient requires treatment for a disability outside the expertise of the clinician, then transferring to a specialist who provides the necessary care may be a more reasonable approach.
- Crisis situations: If you are fired by a patient, then you still may have obligations. You should consider the patient’s state of mind. If the patient cannot make an informed decision, attempt follow-up with the patient or a member of the patient’s support network. Send a letter unless the patient refuses all contact.
- Financial issues: Outstanding account balances should be addressed before the termination option is initiated.
Jurisdictional Considerations
- Federal law: Medical malpractice claims may be brought in the federal courts if diversity of citizenship between the parties exists and the amount of the claim is greater than $75,000.00. Medical malpractice claims also may be brought in the federal courts if the claim raises a federal question or occurs in a federal facility or health clinic.
- State law: State law usually controls medical malpractice claims.
- State licensing board: State licensing boards may have regulations dealing with treatment relationship termination. The State licensing board regulations should be available to all licensed clinicians.
- Case law:
- Warwick v. Bliss: Abandonment is a basis for the physician’s liability to a patient.
- Manno v. McIntosh: Proof of abandonment must include evidence that the physician terminated the doctor-patient relationship in a critical stage of that patient’s treatment, the termination was unreasonable or the doctor gave insufficient notice to allow the patient to find another physician, and injuries flowed to the patient as a result. An explicit point in time marking patient termination is not necessary to prove abandonment. A physician’s failure to see the patient at intervals necessary for proper treatment can constitute abandonment.
CLINICAL SCENARIOS
Scenario #1: A 26-year-old male has stopped taking his atypical antipsychotic and smoked marijuana daily for one month. He lost his insurance six months ago when he turned 26. He has not paid for his monthly visits in five months. He now calls your answering service and says he is suicidal. Must the psychiatrist answer his call?
- In an emergency, a clinician cannot refuse treatment to the patient on the basis of unpaid medical bills but…. The psychiatrist should take the call and follow suicide assessment protocol.
Scenario #2: Dr. Thomas takes two weeks of vacation every Christmas, and the office staff posts a notice online on September 1st every year. A 19-year-old female patient is released from the same hospital that Dr. Thomas leaves as his emergency back up two days before Christmas. The patient calls Dr. Thomas’s answering service, requesting medication. Must Dr. Thomas respond?
- A doctor must be reasonably responsive to a patient. For example, a physician may not go on vacation without leaving emergency coverage or giving reasonable notice to the patient.
ADDITIONAL TIPS
- Treat the patient until a proper termination occurs.
- Style the termination process to the patient. Address the reasons for your decision specific to this patient. Personalize it to reflect the patient’s treatment needs and your recommended follow-up for termination.
- Discuss the end of the relationship with the patient in person, if possible.
- Give the patient notice and reasonable time to find alternative treatment.
- Educate the patient concerning treatment recommendations. Give a reasonable amount of medication for the patient to find a new treatment situation.
- Suggest several resources for treatment.
- Provide records when requested.
- Send a follow-up letter. The letters should include: reason for termination, effective date, interim and continued care provisions, requests for records, patient’s responsibility for follow-up treatments, and medication refills.
- Do not reverse the termination solely because the patient objects to termination.
- Know your state licensing board’s guidelines for termination.
Documentation Tips
- Document all discussions and decisions.
- Keep copies of all prescriptions.
- Keep copies of all the materials. The patient’s record should include the letter, the original certified mail receipt, and the original certified mail return receipt.
REFERENCES
- Terminating the treatment relationship. Psychiatry (Edgemont). 2010 Jan;7(1):40-2. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2848460/pdf/PE_7_1_40.pdf
- Felton EM. Termination: Ending the Therapeutic Relationship-Avoiding Abandonment. Available from: https://naswcanews.org/termination-ending-the-therapeutic-relationship-avoiding-abandonment/
- Brightwell J. Terminating Patient Relationships. Available from: https://www.thedoctors.com/articles/terminating-patient-relationships/
- Medlaw. Avoid Patient Abandonment: 8 Tips for Termination. Available from: https://www.physiciansweekly.com/avoiding-patient-abandonment-proper-termination
- Professional Risk Management Services. Termination of the Psychiatrist-Patient
Relationship. Available from: https://www.prms.com/services/risk-management/termination-of-the-psychiatrist-patient-relationship/ - U.S. Code § 1332. Diversity of citizenship; amount in controversy; costs; Available from: https://www.law.cornell.edu/uscode/text/28/1332
- Bal BS. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009 Feb;467(2):339-47. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2628513/pdf/11999_2008_Article_636.pdf
- Carlson C, Thompson JM. The Role of State Medical Boards. Policy Forum. Virtual Mentor. 2005;7(4):311-314. Available from: https://journalofethics.ama-assn.org/article/role-state-medical-boards/2005-04
- Warwick v. Bliss, 195 N.W. 501 (S.D. 1923).
- Manno v. McIntosh, 519 N.W.2d 815, 821 (Iowa Ct. App. 1994).
- Professional Risk Management Services. Rx for Risk. Available from: https://www.prms.com/media/1662/rx_for_risk_v25_issue2_digital.pdf
Additional Reading
- Gerstner v. Berryhill, 879 F. 3d 257 (7th Cir 2018)
- McNary AL. Myths and Misconceptions: Terminating Treatment. Innov Clin Neurosci. 2021 Jan 1;18(1-3):49-51.